Mark E. McClure, Vasculitis Research Fellow, Addenbrooke’s Hospital, Cambridge
Rachel B. Jones, Consultant in Nephrology and Vasculitis, Addenbrooke’s Hospital, Cambridge
October 2018
Key Points
- Each kidney has approximately one million highly specialised filtering units called glomerlii. Each glomerlius contains a bundle of tiny blood vessels which are very vulnerable to attack in ANCA associated vasculitis.
- Kidney involvement is very common in ANCA associated vasculitis.
- Diagnosis of kidney involvement is made from blood tests, urine tests and often a kidney biopsy.
- Treatment usually involves high dose steroids combined with immunosuppressive medications such as cyclophosphamide or rituximab. In severe cases, a treatment called ‘plasma exchange’ may also be used to help remove ANCA from blood.
- Patients with vasculitis in the kidney may have normal kidney function, or mild-moderately reduced kidney function, or sometimes complete kidney failure (known as end stage kidney disease (ESKD).
- Some patients may need dialysis treatment if their kidney function is too low. This is often temporary as kidney function can improve with prompt treatment for the vasculitis. Unfortunately, the kidney function does not return in some cases and these patients will require either long-term dialysis treatment or a kidney transplant.
Introduction
Vasculitis is inflammation and damage to the walls of various blood vessels. The word vasculitis is derived from the Latin “vasculum” = vessel + “- itis”, inflammation. Another term for vasculitis is angiitis. Each of the vasculitis diseases is defined by certain patterns of distribution of blood vessel involvement, particular organ involvement, and laboratory test abnormalities. ANCA associated vasculitis includes three diseases, each with a rather long name:
- granulomatosis with polyangiitis (GPA, previously called Wegener’s)
- microscopic polyangiitis (MPA)
- eosinophilic granulomatosis with polyangiitis (EGPA, previously called Churg-Strauss)
All three diseases cause inflammation of small blood vessels and are associated with a key protein factor in the blood called ‘ANCA’. Because small blood vessels are found all over the human body, any part of the body can be affected. The kidneys are full of small blood vessels and are the most commonly affected major organ(1).
Where are the kidneys and what do they do?
There are two kidneys in a human body, each about the size of a large potato, located on either side of the spine, just below the rib cage. The major functions of the kidneys are as follows:
- remove waste products from the body in urine
- regulate the body’s fluid balance to prevent dehydration or excess water retention
- release hormones that regulate blood pressure
- produce an active form of vitamin D that promotes strong, healthy bones
- control the production of red blood cells
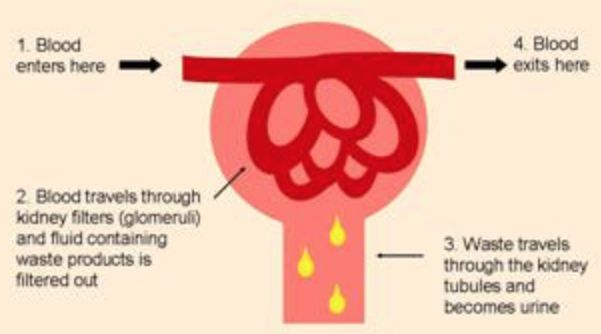
Each kidney contains about a million functioning units called nephrons. A nephron consists of a filtering unit of tiny blood vessels called a glomerulus attached to a tubule. When blood enters the glomerulus, it is filtered (or sieved) allowing small waste products to be release with fluid from the blood, which then passes along the tubule. In the tubule, chemicals and water are either added to or removed from this filtered fluid according to the body’s needs, the final product being urine which flows from the kidney through a pipe called a ureter into the bladder.
How does vasculitis affect the kidneys?
The kidneys are packed with millions of highly specialised tiny blood vessels called glomeruli (pleural for glomerulus). These are very vulnerable to attack in ANCA vasculitis and can become inflamed, swollen and can even burst. This is called glomerulonephritis. When this happens, blood and proteins frequently spill into the urine. Luckily, we have so many glomeruli that we can afford to lose a few without any problems. But if enough glomeruli are damaged, then the overall function of the kidneys is reduced.
How quickly can it progress?
Kidney vasculitis can vary in severity. Some patients have a very aggressive kidney vasculitis known as rapidly progressive glomerulonephritis (RPGN) that can lead to a rapid decline in kidney function and the need for dialysis within days and weeks if left untreated. Conversely, some patients have normal or only very mild reduction in kidney function.
How common is kidney involvement in ANCA vasculitis?
Kidney involvement is very common. It occurs more frequently in MPA (90%) and in GPA (70%) and less frequently in eGPA (25%) (2).
How do I know if the kidneys are involved?
Symptoms
Symptoms of kidney failure are non-specific and often mixed up with other symptoms of vasculitis, including tiredness, lethargy and loss of appetite. There is very little nerve supply to the kidneys so pain is rarely a feature. Some patients may have no symptoms at all.
Signs
Brown, tea-coloured urine from blood leaking into the urine may be seen. However usually the blood in the urine is invisible to the eye and is only identified when urine is tested in the clinic.
Blood tests
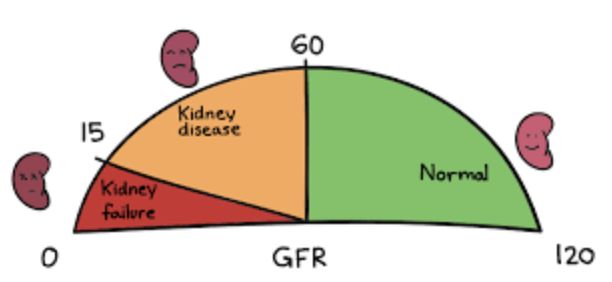
Creatinine is a waste product in your blood that comes from muscle activity. It is normally removed from your blood by your kidneys, but when kidney function is reduced, the blood creatinine level rises. Your doctor may talk to you about creatinine level. Another more accurate measure of your kidney function is Glomerular Filtration Rate (GFR) , which is a calculation that takes into account you age, sex, ethnicity and creatinine and provides as estimated percentage of normal kidney function. More than 60% GFR is considered to be satisfactory. When GFR is less than 10%, dialysis is usually necessary.
Urine tests
Urine can be easily tested in the clinic for several factors including markers of urine infection, sugar (glucose) and for blood and protein. The presence of blood and protein in the urine is abnormal, and should alert doctors to the possibility of active vasculitis or other inflammatory diseases affecting the glomeruli in the kidneys. Urine can be sent to the laboratory for further analysis. Under the microscope the urine red blood cells look ‘dysmorphic’ or misshapen. The actual amount of protein in the urine can be calculated as either protein creatinine ratio (PCR) or albumin creatinine ration (ACR). The amount of blood and protein in the urine usually reduces as the vasculitis is treated, but in some patients, does not go away completely and persists at a low level. Patients with vasculitis normally have their urine tested at each clinic visit to check for changes in the amount of blood and protein in their urine.
Kidney biopsy
If there is any suspicion that vasculitis is affecting the kidneys, a kidney ultrasound scan will usually be performed to check that the kidneys are normal size and shape, followed by a kidney biopsy under local anaesthetic. ANCA vasculitis causes a distinctive pattern of inflammation when examined under the microscope, so not only do biopsies help with the diagnosis of vasculitis, the extent and pattern of inflammation and scarring can be a useful tool in predicting how much improvement in kidney function is likely to occur with treatment, and the likelihood and extent of long-term kidney damage (3).
Treatment of renal vasculitis
The treatment of kidney vasculitis comprises an ‘induction phase’ of 3–6 months to rapidly reduce inflammation and prevent permanent organ damage, followed by a longer ‘maintenance phase, or relapse prevention phase’ once remission has been achieved. Initial induction treatment involves the use of high dose steroids in combination with immunosuppressive drugs; cyclophosphamide and/or rituximab. If the level of kidney function is very low (creatinine >500µmol/l), an additional treatment called plasma exchange is often used. Once remission is achieved, less intensive treatment is used with low dose steroids, and either azathioprine or intermittent rituximab infusions for two years, or longer if a patients is at high risk of relapse.
What about renal relapses?
Relapses in the kidney are identified by the recurrence or increase in level of blood in the urine (usually non-visible – identified on urine dipstick testing) and worsening renal function on blood tests. Fluctuations in the amount of protein in the urine are not good indicators of active disease, and are usually related to chronic damage and scarring. Relapses are treated with the same approach as for a newly diagnosed patient, although rituximab is increasingly being used, to avoid repeated courses of cyclophosphamide.
End Stage Renal Disease (ESRD) and Dialysis
Approximately 20% of patients with renal vasculitis develop end stage renal disease (ESRD) within the few years after diagnosis, which means that they need dialysis and maybe considered for kidney transplantation. A smaller proportion of patients require dialysis immediately when their vasculitis is first diagnosed, of whom approximately 60% will be able to stop dialysis as their kidney function improves with treatment(4). Dialysis is a treatment that removes wastes and excess fluid from the body, either directly from the blood, using a haemodialysis machine (usually in hospital) three times a week or from the fluid in the abdomen every day using peritoneal dialysis at home. The majority of patients with renal vasculitis do not need dialysis because treatments are effective at stopping the vasculitis process, and kidney function shows some improvement in many patients. However, the majority of patients are left with some degree of impaired kidney function known as chronic kidney disease, CKD. Because CKD is associated with high blood pressure and risk of cardiovascular disease, patients with CKD often receive blood pressure and cholesterol lowering tablets.
Predictors of ESRD in ANCA vasculitis
The risk of ESRD is largely determined by the degree of renal impairment at the time of diagnosis. Generally, the higher the initial creatinine level, the greater the chance of reaching ESRD. The worst prognosis is usually seen in patients who required dialysis near diagnosis (6). The kidney biopsy pattern is also a reliable predictor of ESRD. The worst outcomes are associated with a heavy scaring (sclerotic) appearance that is usually accompanied by irreversible kidney impairment. Other risk factors for the development of ESRD include older age, resistance to treatment and renal relapses (7).
Kidney transplantation in ANCA vasculitis
For patients who are fit enough to undergo kidney transplantation, this is a good option for patients with ESRD secondary to renal ANCA vasculitis. However, there are no consensus guidelines on renal transplantation in patients with ANCA vasculitis and practices vary between centres. A survey of transplant centres across Europe identified 107 renal transplant recipients with ANCA vasculitis. All consultants felt that vasculitis should be in remission at transplantation, 16% believed that ANCA should be negative pre-transplant and 40% felt that one should wait >12 months after remission before transplanting. Overall, 70% of the transplants were still working after 10 years (8).
Recurrence of vasculitis in kidney transplants
About 10-15% of patients will have symptoms of vasculitis after a kidney transplant. Not all returning symptoms affect the kidney. Recurrence of vasculitis can occur but rarely cause loss of a transplanted kidney. If you look at all patients with ANCA vasculitis 10 years after their transplant, about 8% of them will have lost their kidney due to recurrence.
Summary
The kidneys are highly specialised organs containing millions of tiny blood vessels that are constantly filtering and regulating the contents of your blood. Unfortunately, these blood vessels are very vulnerable to attack in ANCA vasculitis. Prompt diagnosis and early treatment are the most important factors to improve outcomes. While most patients do not reach end-stage kidney disease, for those that do, kidney function can be supported by dialysis and for patients who are fit enough, renal transplantation is a good treatment option. Overall outcomes continue to improve and the development of more effective, less toxic treatments, undoubtedly will lead to even better outcomes in the future.
- null
- Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013 Jan;65(1):1–11.
- Sinico RA, Di Toma L, Radice A. Renal involvement in anti-neutrophil cytoplasmic autoantibody associated vasculitis. Autoimmun Rev [Internet]. 2013 Feb [cited 2017 Sep 1];12(4):477–82. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22921791
- Berden AE, Ferrario F, Hagen EC, Jayne DR, Jennette JC, Joh K, et al. Histopathologic classification of ANCA-associated glomerulonephritis. J Am Soc Nephrol [Internet]. 2010 Oct 1 [cited 2017 Aug 31];21(10):1628–36. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20616173
- Moiseev S, Novikov P, Jayne D, Mukhin N. End-stage renal disease in ANCA-associated vasculitis. Nephrol Dial Transplant [Internet]. 2016 Apr 6 [cited 2017 Sep 1];24((1 Suppl 70)):gfw046. Available from: https://academic.oup.com/ndt/article-lookup/doi/10.1093/ndt/gfw046
- de Lind van Wijngaarden RAF, Hauer HA, Wolterbeek R, Jayne DRW, Gaskin G, Rasmussen N, et al. Chances of renal recovery for dialysis-dependent ANCA-associated glomerulonephritis. J Am Soc Nephrol [Internet]. 2007 Jul 1 [cited 2017 Aug 31];18(7):2189–97. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17596637
- Lionaki S, Hogan SL, Jennette CE, Hu Y, Hamra JB, Jennette JC, et al. The clinical course of ANCA small-vessel vasculitis on chronic dialysis. Kidney Int [Internet]. 2009 Sep [cited 2017 Sep 1];76(6):644–51. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19536079
- Sinico RA, Di Toma L, Radice A. Renal involvement in anti-neutrophil cytoplasmic autoantibody associated vasculitis. [cited 2017 Sep 1]; Available from: http://pneumonologia.gr/articlefiles/Renal involvement in anti-neutrophil cytoplasmic autoantibody associated vasculitis.pdf
- Little MA, Hassan B, Jacques S, Game D, Salisbury E, Courtney AE, et al. Renal transplantation in systemic vasculitis: when is it safe? Nephrol Dial Transplant [Internet]. 2009 Oct 1 [cited 2017 Sep 1];24(10):3219–25. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19602476
