Professor Alan Salama
Professor of Nephrology and Honorary Consultant Nephrologist Royal Free Hospital London
February 2019
What is Polyarteritis Nodosa?
Polyarteritis Nodosa (PAN) is a very rare relapsing vasculitic disease which affects medium sized blood vessels, such as those supplying the kidneys and bowel.
It can affect all ages although there may be differences in the main symptoms between children and adults. Men and women are almost equally affected.
PAN was a term first used to describe various forms of vasculitis, but with better understanding of the causes and associations of the disease we can now sub-classify the condition, which helps with its management, defining the likely outcomes, counselling of patients and relatives and initiating the most appropriate treatment. It may be that these subtypes are really different diseases, but with some similar clinical features which occur when medium sized blood vessels are damaged by various biological factors, and the more we understand about the causes, the better we will understand their relationships.
What are the symptoms?
It depends on the area affected and it can, like most forms of vasculitis, affect any organ in the body, but common symptoms include weight loss, muscle aches, joint pains, skin rashes or nodules, abdominal pains, sometimes with blood in the stools, and numbness or tingling in the hands or feet. Less often eye problems, breathing difficulties chest pains, or pain in the testicles can occur. In certain forms of PAN strokes occurring at a young age are common. Kidney involvement and high blood pressure is also often found but may be without symptoms.
Table: Common symptoms in children and adults with PAN according to frequency
| Symptoms | Adults | Children |
| Most Frequent | Nerve involvement | Skin –rashes, nodules, ulcers |
| Skin –rashes, nodules, ulcers, muscle aches, weight loss | Fever, joint pains, muscle aches | |
| Joint pains, fevers | Nerve involvement | |
| Less frequent | Abdominal pains, high blood pressure, kidney damage | Weight loss, Abdominal pain, kidney damage, high blood pressure |
PAN Subtypes and associations:
- Infections: PAN can be associated with Hepatitis B virus infection, and less commonly with other viral infections such as HIV or Hepatitis C. There may be a known history of contracting/carrying these infections.
- Genetic diseases: PAN may be associated with inherited (genetic) forms of periodic fever syndromes, in particular a condition called Familial Mediterranean Fever (FMF), which is especially common in patients from the Eastern Mediterranean. In this form, abdominal pains, muscle aches and bleeding around the kidney are common features. Other genetic diseases which result in a PAN-like disease are found in patients with defects in a gene termed DAD2. In this form joint pains and strokes are common.
In all these genetic cases there may be a family history of similar problems, although not always in immediate family members (parents, siblings, or grandparents), as the condition may be recessively inherited, so sometimes generations may be skipped. - Classical PAN: In those without an obvious (currently known) association we call them classical PAN.
- Cutaneous PAN: This is a limited form of PAN that at least initially is confined to the skin. It seems that cutaneous PAN doesn’t often lead to more widespread PAN, but there may be some limited symptoms apart from the skin problems. Some forms of cutaneous PAN may be related to exposure to particular drugs(such as minocycline , an antibiotic)
- PAN associated with other autoimmune rheumatic diseases: medium vessel vasculitis can be found in other rheumatic diseases such as Sjogren’s syndrome, and rheumatoid arthritis although these may be separate autoimmune diseases in the same patient or manifestations of a single rheumatic disease.
We therefore now qualify what form of PAN it may be, for example Hepatitis B associated PAN, FMF-PAN, classical-PAN or DAD2- PAN, and bearing in mind that we may discover new associations or causes in the future.
PAN is always ANCA negative, and the finding of ANCA in a patient suggests a different form of vasculitis (see ANCA associated vasculitis).
Who are affected?
Classical PAN is most common in middle age, but adults and children can have this disease. Many of the older series describing PAN did not adequately differentiate all the new forms and subtypes as they were not known about, with the exception of Hepatitis B associated PAN. As a result what we know about the particular subtypes is only now being truly appreciated.
What causes PAN?
The cause of classical or cutaneous PAN is not yet known. There is an attack on the blood vessel wall by the patient’s own immune system. Why certain blood vessels are affected and in certain areas, and what provokes the autoimmune attack is still not clear. In those people with PAN and Hepatitis B virus infection, the reason for the blood vessel damage is also uncertain. Only a very few people with hepatitis B infection ever develop PAN and only a small proportion of people with PAN have hepatitis B infection. This form of PAN is becoming significantly less common as a result of vaccination for and treatment of hepatitis B infections.
Diagnosis
As with other types of vasculitis there is no one single diagnostic test.
Diagnosis is based on the symptoms described by the patient, physical examination, various laboratory tests (to exclude other causes of the symptoms and point to PAN) and possibly biopsy of the affected area. In the genetic forms of disease, specific genetic tests are required to make the right diagnosis.
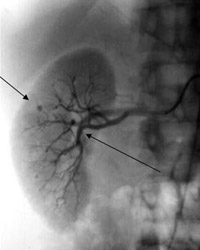
Blood tests will show evidence of inflammation. The blood vessels in the abdomen are commonly affected and angiography (x-rays of the blood vessels- see Figure) can show typical findings which help with the diagnosis. It is important to test patients with PAN for hepatitis B virus, HIV and Hepatitis C as these may require separate treatments.
Treatment
For classical PAN, high dose steroids and cyclophosphamide are often used to get the inflammation under control. Once under control treatment is often continued for 12 months using steroids and other immunosuppressants such as azathioprine, and then can be stopped in some patients. Disease relapses do occur and in some cases longer duration of remission treatment may be needed.
Patients with infectious causes will need specific treatment for the particular infections with anti-viral drugs, usually under specialist care. For certain subtypes of PAN there may be other specific treatments – for example colchicine works well in suppressing the inflammation in FMF-PAN, while anti-TNF therapies, sometimes used in rheumatoid arthritis, are most effective in DAD2 associated PAN.
Drugs and Side effects
For information on the main drugs prescribed for Polyarteritis Nodosa see:
- Cyclophosphamide
- Steroids
- TNF blockade
For information on other drugs used in the treatment of vasculitis see Glossary of drugs and side effects
Prognosis
With treatment the prognosis is generally good. In most cases treatment can be stopped after 12 months. In some patients the disease relapses requiring longer term treatment.
Key Points
- PAN is a rare type of vasculitis
- There are many different forms of what we call PAN
- It is known to be associated with various other conditions including hepatitis B virus infection
- Treatment depends on the severity and subtype of PAN
Further reading
- Michael J Dillon, Despina Eletheriou, Paul A Brogan: Medium-size Vessel Diseases. Paediatric Nephrology 2010
- Sonmez HE et al .Polyarteritis nodosa: lessons from 25 years experience Clinical Experimental Rheumatology 2018
- Karadag and Jayne: Polyarteritis nodosa revisited:a review of historical approaches, subphenotypes and a research agendaClinical and Experimental Rheumatology 2018
- Lucidi et al Childhood versus adult onset polyarteritis nodosa: results from the French vasculitis study group registry. Autoimmunity reviews 2018
