The Trust is indebted to Dr Marcos Martinez del Pero, Specialist Registrar in ENT, East of England Deanery, Cambridge, UK for providing the following information on vasculitis and the ear
Vasculitis can either affect the ear as part of a general illness, for example in Wegener’s granulomatosis (now called granulomatosis with polyangiitis –GPA-), or can be a localised problem, for example autoimmune hearing loss. Problems with the ear can come before other features of disease in GPA and correct diagnosis is important in order to prevent hearing loss and more widespread illness. This article will discuss the different ways in which vasculitis can affect the ears and the different treatments available.
Ear anatomy and function
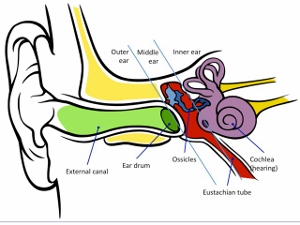
It is worth starting by explaining the different names doctors give to parts of the ear (Figure 1) and the different types of hearing loss. The outer ear extends from the part that one can see up to the eardrum. The middle ear is the space between the eardrum and the skull, it contains the hearing bones or ossicles (malleus/mallet, incus/anvil and stapes/stirrup) and it is drained by the Eustachian tube. The inner ear forms part of the bone of the skull where the sound is converted into electric stimuli for transmission by nerves to the brain. Next to it are the semicircular canals and the rest of the balance organ.
In terms of hearing loss it is divided into ‘conductive loss’, when the ear drum and/or the ossicles are affected; and ‘sensorineural loss’ when the cochlea, the nerve and/or the hearing centre in the brain are affected. In some cases the hearing loss is a mixture of conductive and sensorineural loss.
How is vasculitis diagnosed in the ear?
Patients who present with vasculitis, which is limited to the ear, often have the same symptoms and show the same appearances as patients with infections and congestion in the middle ear. Very occasionally they have inflamed tissue behind the eardrum (Figure 2B). Another way vasculitis patients present is with sudden (over less than three days) nerve hearing loss.
The features that would point towards a diagnosis of vasculitis are an infection that does not respond to optimal treatment, greater pain than appearance of the ear would suggest and inflammatory tissue filling the middle ear. All patients that suffer from acute sensorineural hearing loss are treated with steroids. If the hearing responds well, an inflammatory process such as vasculitis is suspected, particularly if the hearing drops again on another occasion.
All patients suspected of GPA should have a urine dipstick done in the clinic and a chest x-ray as well as blood tests that include ANCA. However, in conditions such as Churg-Strauss syndrome (now called eosinophilic with polyangiitis –EGPA-) or limited GPA, these tests may not be helpful and biopsies may be required. The difficulty is that biopsies are often negative because vasculitis or granulomas may not be seen in the sample and what is seen could be caused by a number of inflammatory conditions. In these cases, close monitoring and repeat testing is required and occasionally treatment is started before having positive tests based on clinical findings.
How do different forms of vasculitis affect the ear?
Granulomatosis with polyangiitis (Wegener’s granulomatosis)
Acutely, patients may present with a painful discharging ear, infection or deafness. They often have nasal symptoms as well, that cause scarring of the Eustachian tube and congestion behind the eardrum. Some of these patients may have grommets (ventilation tubes through the ear drum) inserted that unfortunately, can result in constant ear discharge and little relief of deafness or discomfort.
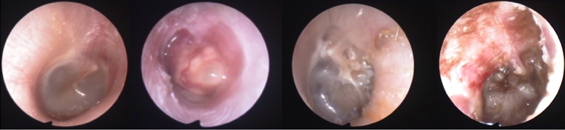
During remission up to 60% of patients with GPA have involvement of the ears. Their complaints include persistent/recurrent discharge and hearing loss. The abnormalities seen when examining the eardrums are shown in Figure 2. The type and level of hearing loss seen in GPA is usually different in each ear and does not have a characteristic pattern seen in other conditions (for example with increasing age we tend to see patients with hearing loss that affects the same frequencies in both ears)
Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome
Ear disease in EGPA, can be also limited to the ears or part of a widespread disease. The symptoms are similar to those seen in GPA, but these patients seem to have a higher incidence of chronic inflammation in the middle ear and pain in the middle ear. The appearances and type of hearing loss is the same as that seen in GPA i.e. no characteristic pattern.
Microscopic polyangiitis
Patients with this type of ANCA vasculitis do not suffer from the destructive effects that GPA patients do. However, they may develop sensorineural hearing loss as a consequence of inflammation of the small vessels supplying the hearing nerve.
Other symptoms
There are other symptoms that can affect the ear, but they are considerably less common and are not associated with a particular type of vasculitis or in most cases with a vasculitic process. These include tinnitus (a sensation of sound in the ear without a stimulus) and vertigo. Tinnitus can affect anyone, but it is often associated with hearing loss. Vertigo takes many forms and the different inner ear pathologies present in the same way as in the general population. Rarely vasculitis can affect the nerve of the inner ear balance organ and cause similar symptoms to labyrinthitis (nausea and vomiting and a sensation of movement that lasts for a few days).
How is it treated?
Once the diagnosis is made, the initial treatment consists of systemic immunosuppression either with steroids alone or with immunosuppressants such as cyclophosphamide or methotrexate.
Conservative
Infections with ear discharge with or without a hole in the eardrum are treated antibiotic drops. If the infection is not settling or the canal is full of pussy discharge, the treatment involves cleaning the ear with suction in the ENT clinic and antibiotic creams or different antibiotic drops. If the infection is in the middle ear and does not settle on its own, it may require oral antibiotics. The treatment is expected to work within a week, but in the case of deep infections it may take a few weeks of intense treatment. However, one should consider low-grade activity if the infections do not settle as expected.
Hearing aids are useful in patients with conductive (middle ear problems) or sensorineural hearing loss (‘nerve’ hearing loss). Patients with constant ear discharge, who require aiding, may benefit from implantable devices. Hearing aids can also be helpful in patients with very intrusive tinnitus and if the patient has hearing loss, they are the first line of treatment. In patients whose tinnitus does not let them sleep or concentrate a referral to a specialist in tinnitus may be helpful. The specialists are usually audiologists who will try and find the trigger, provide information and sometimes white noise devices.
Surgical
Generally surgery is avoided in patients with vasculitis, but in patients who have been in remission for over 12 months and have a persistent discharge, surgery to repair the eardrum may be considered appropriate. In patients with congestion in the middle ear (glue ear) who are also in remission, a ventilation tube (grommet) may be helpful. There is not much evidence to inform the management decisions, so each individual case is considered with the advice of the medical team. In addition, patients may suffer from conditions affecting the rest of the population, such as, cholesteatoma (a condition where the ear drum retracts into the middle ear and traps skin within it). In these cases surgery should be considered with the advice from the medical team on medications before, during and after surgery.
Outcome
Nerve related hearing loss can recover with corticosteroids in some cases, particularly when treated within a few days, but in most cases it does not recover completely. Conductive hearing loss usually implies damage to the eardrum or the ossicles or congestion behind the eardrum. If there is only glue ear with no other damage, grommets can potentially return the hearing to normal or to the level the nerve functions. If a more extensive procedure to repair the eardrum or the ossicles is required, the chances of improved hearing to normal levels are lower (between 50-80% will benefit five years after the surgery). The chance of repairing the eardrum successfully is quoted as 85% in the general population, but there are no published case series in vasculitis.
Regarding tinnitus, most the time the brain learns to ignore it and it becomes part of the background noise. In patients whose tinnitus is very intrusive the therapies mentioned above can aid the process of reducing the tinnitus to the background.
Is there anything I can do to protect my hearing?
For patients who suffer from chronically discharging ears it is advisable to cover the opening of the ear canals with cotton wool smeared in Vaseline during showers or baths. If the patient is a keen swimmer personalised swimming moulds can be helpful. Cotton buds do not help to clean the ears and often cause more harm by traumatising the ear canal or pushing wax deep in the ear canal. No harm is done by using or not using hearing aids, but if people become withdrawn because they cannot follow a conversation, then this might be a good time
