formerly Wegener’s Granulomatosis
Reviewed and revised by:
Dr Chetan Mukhtyar MBBS, MSc, MD, FRCP, FRCPE
Consultant Rheumatologist
Norfolk and Norwich University Hospital
February 2023
Change of nomenclature
The name of this vasculitic disease was officially changed from Wegener’s Granulomatosis (WG) to Granulomatosis with Polyangiitis (GPA) in 2011. Throughout this descriptive section it will be referred to as GPA.
What is Granulomatosis with Polyangiitis?
GPA is a type of primary systemic ANCA associated vasculitis (AAV). It is the most common type of this group of vasculitis diseases. It usually affects the kidneys, lungs, ears, nose and sinuses. GPA is characterised by inflammation of the small blood vessels including the capillaries.
Who are affected?
It is most common in middle aged and elderly people but can affect young adults and children. It affects men and women equally.
What is the aetiology (cause)?
The cause of GPA is not yet known. Some research suggests that GPA may be triggered by exposure to silica or to infection with staphylococcus aureus bacteria though this is not proven.
The ANCA antibodies found in most patients with GPA play a role in causing the inflammation of the blood vessels by activating some types of white blood cell. The ANCA antibodies attach to the neutrophils in the blood causing activation. This makes the neutrophil attach to the blood vessel wall and cause damage by release of the chemicals that it usually uses to fight infection. It is not understood why patients develop ANCA antibodies.
What are the symptoms?
The disease can present in very different ways in different people depending on the severity and the organs involved. It is not uncommon for patients to have had mild symptoms for months or even years before seeing a doctor at all.
Common general symptoms include tiredness, loss of appetite and aching muscles and joints.
It is very common for GPA to affect the ears, nose and sinuses causing blocked nose with some bleeding, crusts and blood clots. Deafness is also very common due to inflammation in the ears as is pain in face or headaches due to sinus inflammation. The eyes can also be involved.

In some patients the kidneys can be severely affected which leads patients to go to a doctor with symptoms of kidney disease.
Other common symptoms include:
- Lungs – breathlessness, wheeze, dry cough or coughing up blood
- Skin – rashes, ulcers, and necrosis (death of tissue)
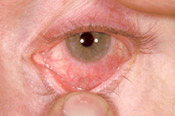
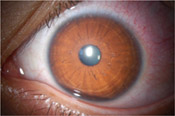
- Eyes – red (blood shot) eyes, painful, dry or gritty eyes, visual loss or other changes in vision
- Nerves – loss of sensation, weakness, unusual painful symptoms in the hands and feet
- Bowels – Diarrhoea, bleeding and abdominal pain.


Diagnosis
As in other types of vasculitis there is no single test which confirms the diagnosis. The diagnosis will depend on the doctor recognising the pattern of symptoms and examination findings. Blood tests usually show evidence of inflammation. The blood tests for ANCA are usually positive which help support the diagnosis but are not specific for GPA or vasculitis A biopsy of the affected organ (if readily accessible) may be helpful in confirming the diagnosis The affected organ may not always be readily conducive to a biopsy. For example brain or eye involvement are best not biopsied, whereas kidney or nose involvement are easily biopsied. GPA can often present with nonspecific symptoms of unwellness, fever, malaise and may mimic infections, making it difficult to diagnose. If the lungs are primarily affected it is not uncommon for the disease to be mistaken for lung cancer, pneumonia or TB.


Treatment
Cyclophosphamide or Rituximab in combination with glucocorticoid (steroids) are the main treatment options in most cases. In specific circumstances, methotrexate or mycophenolate mofetil may be of value. If the disease is very severe, large doses of methylprednisolone or plasmapheresis (plasma exchange) may also be given.
When the disease becomes quiet, less toxic drugs are used to keep control which include: azathioprine, methotrexate and mycophenolate mofetil. In patients where initial treatment was with rituximab, it may be continued in a smaller dose at 4-6 monthly intervals. The prednisolone will be tapered slowly over time with a view to coming off the steroid completely. In some cases, this may not be possible and a low-dose of prednisolone may have to be continued long-term.The treatment will be continued for at least two years after the onset of remission after which it may be appropriate to start reducing it in certain cases.
For information on plasma exchange:
Drugs and Side effects
For information on the main drugs prescribed for GPA see:
For information on other drugs used in the treatment of vasculitis see Glossary of drugs and side effects.
Prognosis
The overall prognosis in GPA depends on the amount of damage that has been done to organs, especially the kidneys, when the disease was active. Relapses are common and can occur in up to 40% of patients at 2 years after remission. Your doctor will have to change your immunosuppressive treatment in the event of a relapse. In very few cases, it may be reasonable to simply increase or commence a small dose of prednisolone (steroids).
Key Points
- GPA is the most common type of this group of vasculitis diseases
- The disease may be present for months or years before a diagnosis is made
- Treatment depends on the severity of the disease
- The disease commonly relapses after the initial treatment.
Related Vasculitis Articles
- Fertility and Vasculitis – Dr David Jayne
- Vasculitis and the Ears – Dr Marcos Martinez del Pero
- Vasculitis and the Eyes – Dr Catherine Guly
- Vasculitis in Children – Dr Paul Brogan
Further reading
- Recommendations on the use of Rituximab in ANCA-associated Vasculitis – Rheumatology 2012
- Classification, presentation, and initial treatment of Wegener’s granulomatosis in childhood– David A Cabral, America G Uribe, Susanne Benseler, et al
- Small Vessel Vasculitis – Paul Brogan, Despina Eletheriou, Michael Dillon
- Management of ANCA-associated vasculitis: Current trends and future prospects – Sally Hamour, Alan D Salama, Charles D Pusey
- Vasculitis Paediatric Guidelines 2012 – Dr Helen Foster & Dr Paul Brogan, Oxford University Press
- Nose Reconstruction in the Individual with Systemic Vasculitis – The Centre for Nose Reconstruction at Poole Hospital
- EULAR/ERA-EDTA recommendations for the management of ANCA-associated Vasculitis July 2016
