Churg Strauss Syndrome
now renamed
Eosinophilic Granulomatosis with Polyangiitis (EGPA)
Dr Thomas Jones (Wessex Research Fellow)
Respiratory Department, Portsmouth Hospitals NHS Trust, supported by Professor Anoop Chauhan (Respiratory Consultant and Director of Research and Innovation) Portsmouth Hospital NHS Trust
October 2015
What is EGPA?
Eosinophilic Granulomatosis with Polyangiitis (EGPA), previously known as Churg-Strauss Syndrome, is an inflammatory disease of small and medium sized blood vessels. The lungs and skin are commonly affected but it can affect other organs including the heart, kidneys, nerves and bowels.
Eosinophils, a type of white blood cell that typically fights parasite infections and is related to allergies, are found in very high levels in EGPA, both in blood tests and in affected parts of the body.
Who is affected?
EGPA seems to affect men and women equally. Around 11-13 people per million are diagnosed with EGPA. The average age of someone with a new diagnosis is 40 years old, and it is very rare in children or those over 65 to be diagnosed.
What is the aetiology (cause)?
The cause of EGPA is not known. It is likely that a combination of factors lead to development of EGPA. Studies looking at genetics have shown some genes that are linked to EGPA, while some people have Anti Neutrophil Cytoplasmic Antibodies (ANCA) which may cause some types of auto-immune disease. Unusual levels of some types of hormone-like chemicals in the blood (cytokines) have also been found in people with EGPA, and this may contribute too.
What are the symptoms?
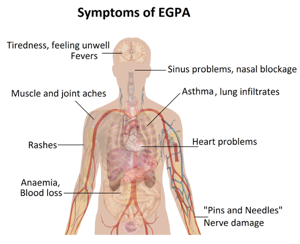
People who suffer with EGPA usually have severe asthma that may have developed as an adult. They often have sinus and nose symptoms and may have a number of other symptoms including: rashes, nerve damage including pins and needles or numbness, bowel trouble and blood loss, anaemia, heart problems, muscle and joint pain and tiredness. Symptoms often develop in phases:
First “prodromal” phase – People with EGPA often suffer allergies, asthma and sinus symptoms starting in their teens and twenties.
Second “eosinophilic” phase – High levels of eosinophils are found in blood tests, and often in affected organs.
Final “vasculitic” phase – Inflammation of small and medium vessels (vasculitis) begins, often in the twenties and thirties. Symptoms of tiredness, weight loss and fever often precede this.
How is it diagnosed?
The most up to date diagnostic rules, written by the European Respiratory Society (ERS), say that someone with EGPA should have:
- Asthma
- High levels of eosinophils in the blood (over 10% of all white blood cells)
- Damage from vasculitis to the skin, nerves, kidney, lung, heart or blood tests suggesting vasculitis
The ERS also suggested a sub-type of EGPA called Hypereosinophilic Asthma with Systemic Manifestations (HASM), where vasculitis itself was not present, but patients had other types of organ damage from eosinophils.
Diagnostic tests
Blood tests – Blood tests will show high levels of Eosinophil white blood cells in patients with active EGPA. Blood tests may also show damage to the kidneys, or may show a type of antibody related to vasculitis (ANCA).
Chest X-ray – People with active EGPA may have patches of vasculitic damage where eosinophils invade and damage the lung tissue (infiltrates) that may be visible on a chest x-ray.
Lung function – All patients diagnosed with EGPA have asthma, and this will almost always be shown through spirometry (breathing tests) that show an inability to breathe out a quickly as should be possible which improves when given inhaled treatment.
Biopsy – If biopsies (tissue samples) are taken, these may show high numbers of eosinophils, collections of immune cells (known as a granuloma), and damage to blood vessels cause by immune cells (vasculitis). Biopsies may be taken from any affected tissues (lung, nerves, skin, kidneys etc.) and are the most conclusive way of diagnosing the disease.
Bronchoscopic lavage – Camera tests may be performed to “wash out” areas of the lung. This fluid can show high numbers of eosinophils and may have blood in too. This test is most useful in making sure that other problems such as infection or cancers are not present.
Heart tests – People with EGPA can have damage to their heart, and so a heart tracing (electrocardiogram – ECG) and/or ultrasound test (echocardiogram) are often performed. This may be followed up with further tests where abnormal areas are found.
Treatment options
Corticosteroids – Steroids like prednisolone form the backbone of treatment of people with EGPA. Steroids are often needed at quite high levels initially, and should be tapered off although this can take many years. Reduction of steroid treatment should be done very carefully as dropping steroid levels too quickly can result in EGPA becoming more active or not having enough steroid within the body. Steroids can have multiple side effects – see page on corticosteroids.
Nasal and inhaled steroids – As well as steroid tablets, people with EGPA often need steroid sprays to treat their nose and sinus symptoms. These can help people breathe through their nose more easily and try to preserve their sense of smell. Steroid inhalers are used to control the asthma that almost all people with EGPA experience and prevent worsening of their breathing.
Cyclophosphamide – In people with severe EGPA and those who do not respond well to steroid treatment, medication like cyclophosphamide may be used. This can be given by mouth or into veins, and is continued for a limited period of time. See page on cyclophosphamide.
Azathioprine – Azathioprine is sometimes added into treatment for people who are struggling to reduce their level of steroids without their EGPA becoming more active. Blood tests are needed before starting azathioprine as some people react very badly to it.
Methotrexate – used similarly to azathioprine, methotrexate is sometimes used to help with reduction in steroid treatment.
Rituximab – A new injection treatment, Rituximab is occasionally used in severe EGPA that has not responded well to other treatment.
Other medications – New medication including other injectable antibody treatments are being researched and may become available over the next few years.
Alternative medicine – There is no evidence that any types of alternative medicines are useful in EGPA, and they should not be used in place of medical treatment.
Prognosis
Before treatment for EGPA was available, it was universally fatal. Half of patients diagnosed with EGPA died within 3 months of diagnosis. With modern treatment, this is much improved. We think that 8 in every 10 people diagnosed are still alive 5 years later. People who have involvement of the heart, kidneys, gut and brain seem to be at higher risk and may require more intensive treatment to prevent complications.
Related Vasculitis Articles
- Fertility and Vasculitis – Dr David Jayne
- Vasculitis and the Ears – Dr Marcos Martinez del Pero
- Vasculitis and the Eyes – Dr Catherine Guly
- Vasculitis in Children – Dr Paul Brogan
Further reading
- Recommendations on the use of Rituximab in ANCA-associated Vasculitis – Rheumatology 2012
- Churg-Strauss Syndrome: Evolving Concepts – Christian Pagnoux
- Small Vessel Vasculitis – Paul Brogan, Despina Eletheriou, Michael Dillon
- Small vessel and medium vessel vasculitis – Philip Seo, John H Stone
- Management of ANCA-associated vasculitis: Current trends and future prospects – Sally Hamour, Alan D Salama, Charles D Pusey
- Guidelines for the management of adults with ANCA associated vasculitis – (Rheumatology 2007;46:1-11)
- Vasculitis Paediatric Guidelines 2012 – Dr Helen Foster & Dr Paul Brogan, Oxford University Press
Useful links
Our Useful Vasculitis Links page contains contact details for organisations offering help and support for patients with Churg Strauss Syndrome (EGPA) and other vasculitis diseases.
Personal story
You can read one person’s experience of Churg Strauss Syndrome at: Emma’s story
This page was updated in April 2016
